Allergy
Blood Diseases
Bone & Joints
Brain
Cancer
Child Care
Cosmetic Surgery
Diabetes
Endocrinology
ENT
Eye
Gen Medicine
General Surgery
Heart
Kidney
Lifestyle
Liver & Digestive
Lung
Men’s Health
Mental health
Physiotherapy
Rheumatology
Skin and hair
Sleep Disorders
Spine
Transplant
Women Health
Thyroid
Vascular Surgery
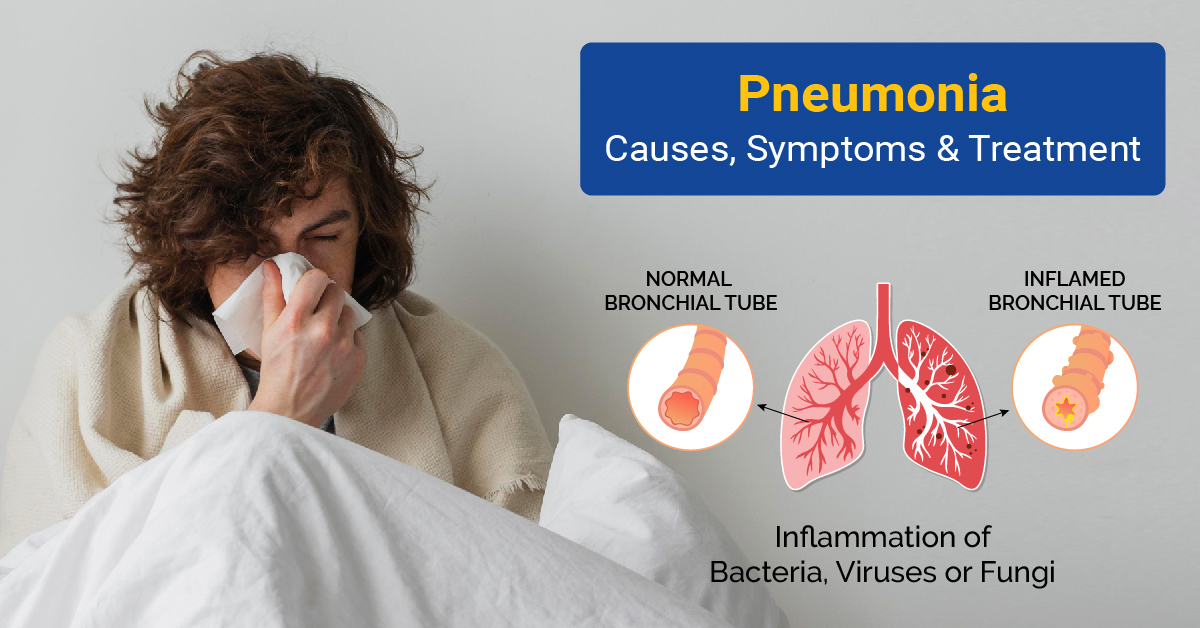
Pneumonia Symptoms and Diagnosis
Introduction
Pneumonia, a respiratory infection affecting the lungs, can be a serious health concern if left untreated. Understanding the causes, identifying symptoms, and knowing the available treatment options are crucial for effective management. This comprehensive guide will delve into the various aspects of pneumonia, from its diverse causes to treatment modalities and preventive measures.
Causes of Pneumonia
Understanding the source of infection is crucial for tailoring appropriate treatment plans. Bacterial pneumonia, for instance, is typically treated with antibiotics, while viral pneumonia may require antiviral medications.
Pneumonia, an infection affecting the lungs, can cause inflammation and fluid or pus accumulation within the tiny air sacs (alveoli). This can lead to difficulty breathing, cough, fever, and other symptoms. Understanding pneumonia - its causes, symptoms, diagnosis, treatment, and prevention is crucial for managing this potentially serious condition.
Causes of Pneumonia: Exploring the various origins
Several microorganisms can cause pneumonia. The most common ones include:
- Bacteria: Streptococcus pneumoniae and Haemophilus influenzae are the leading bacterial culprits, causing typical "bacterial pneumonia."
- Viruses: Respiratory viruses like influenza, rhinovirus, and respiratory syncytial virus (RSV) are common causes of "viral pneumonia," often milder than bacterial pneumonia.
- Fungi: Certain fungus varieties like Pneumocystis jirovecii can cause "fungal pneumonia," primarily affecting people with weakened immune systems.
- Other less common causes include Mycoplasma pneumoniae, Chlamydia pneumoniae, and aspiration pneumonia (inhalation of foreign substances like food or vomit).
Pneumonia can be caused by various pathogens, with viral, bacterial, and fungal origins being the primary culprits. Viral pneumonia often stems from influenza viruses, respiratory syncytial virus (RSV), and adenoviruses. On the other hand, bacterial pneumonia is commonly caused by Streptococcus pneumoniae, Haemophilus influenzae, and Staphylococcus aureus. Fungal pneumonia is rare but can occur in individuals with compromised immune systems, caused by fungi such as Pneumocystis jirovecii.
Symptoms Identification
Recognizing the symptoms of pneumonia is essential for prompt intervention. Common signs include persistent cough, difficulty breathing, chest pain, and fever. Patients may also experience fatigue, confusion, and bluish discolouration of the lips or nails, indicating a lack of oxygen.
Symptoms of pneumonia can vary depending on the cause, severity, and individual health. Some common signs and symptoms include:
- Cough: This is the most common symptom, often productive, which brings up phlegm (mucus) that may be yellow, green, or bloody
- Fever: Elevated body temperature, usually accompanied by chills and sweating
- Shortness of breath: Difficulty breathing, especially noticeable during physical activity
- Chest pain: Pain or tightness in the chest, often worsening when breathing deeply or coughing
- Fatigue: Feeling tired and weak, with decreased energy levels
- Other symptoms: Headache, muscle aches, loss of appetite, nausea, and vomiting
- In infants and young children, symptoms may be less specific, including poor feeding, lethargy, and irritability
Early detection can significantly improve outcomes, making it vital for individuals to seek medical attention if they exhibit these symptoms. It is especially important for vulnerable populations, such as the elderly, young children, and those with weakened immune systems, to be vigilant about respiratory distress.
Diagnostic Procedures
Accurate diagnosis is crucial for determining the specific cause of pneumonia and tailoring appropriate treatment.
Several tests and procedures aid in diagnosing pneumonia:
- Physical examination: Doctors listen to the lungs with a stethoscope to detect abnormal breath sounds.
- Chest X-ray: This imaging test provides a visual representation of the lungs and can reveal areas of infection.
- Blood tests: These tests can confirm infection and determine the type of pneumonia.
- Sputum culture: A sample of phlegm is analyzed to identify the specific bacteria causing the infection.
- Pulmonary function tests: These tests measure lung function to assess the severity of the infection.
The specific tests chosen depend on the severity of symptoms, age, and underlying medical conditions.
Healthcare professionals employ various diagnostic procedures, including chest X-rays, blood tests, and sputum cultures. Chest X-rays can reveal the extent and location of lung inflammation, aiding in distinguishing between viral and bacterial pneumonia. Blood tests help identify the causative agent by detecting specific antibodies or antigens. Sputum cultures involve analyzing mucus coughed up from the lungs to pinpoint the responsible pathogen.
These diagnostic tools collectively contribute to a comprehensive understanding of the infection, guiding healthcare providers in formulating an effective treatment plan.
Treatment Modalities
The treatment approach for pneumonia depends on the cause and severity. Common treatment options include:
- Antibiotics: These medications are the primary treatment for bacterial pneumonia. The specific type of antibiotic chosen is based on the bacteria identified
- Antiviral medications: These medications may be used for severe cases of viral pneumonia
- Antifungal medications: These medications are used to treat fungal pneumonia
- Over-the-counter medications: Pain relievers like ibuprofen or acetaminophen may be used to manage fever and pain
- Rest: Getting adequate rest is crucial for recovery
- Hydration: Drinking plenty of fluids helps thin mucus and prevent dehydration
- Supportive care: Oxygen therapy may be needed to improve oxygen levels in severe cases
Sometimes, hospitalization may be necessary for close monitoring and intensive treatment.
The treatment of pneumonia depends on its underlying cause. Bacterial pneumonia is commonly treated with antibiotics, which target and eliminate the bacteria responsible for the infection. It is crucial for patients to complete the entire course of antibiotics, even if symptoms improve, to prevent the development of antibiotic-resistant strains.
Viral pneumonia, being caused by viruses, may not respond to antibiotics. Antiviral medications may be prescribed in these cases, focusing on inhibiting the virus's ability to replicate and spread. Supportive care, including rest, adequate hydration, and over-the-counter pain relievers, can help alleviate symptoms and aid recovery. For fungal pneumonia, antifungal medications are the primary mode of treatment.
It is imperative for individuals with compromised immune systems, such as those with HIV/AIDS or undergoing chemotherapy, to follow their healthcare provider's recommendations closely.
Preventive Measures
Preventing pneumonia involves a combination of vaccination and hygiene practices. Vaccination is a key preventive measure, particularly for bacterial pneumonia. In addition to vaccination, practicing good hygiene is essential. Regular handwashing, avoiding close contact with sick individuals, and maintaining a clean living environment can help reduce the risk of respiratory infections. Several steps can be taken to prevent pneumonia:
- Vaccination: Getting vaccinated against influenza, pneumococcus, and other respiratory viruses significantly reduces the risk of pneumonia.
- Good hygiene practices: Regularly washing hands with soap and water or using hand sanitizer helps prevent the spread of germs.
- Smoking cessation: Smoking damages the lungs and increases the risk of pneumonia.
- Maintaining a healthy lifestyle: Eating a healthy diet, exercising regularly, and getting enough sleep can boost immunity and overall health.
- Avoiding crowds and sick individuals: This reduces the risk of exposure to infectious agents.
Individuals with underlying health conditions and those in high-risk groups need to prioritize preventive measures.
Conclusion
Pneumonia, with its diverse causes and potentially severe consequences, demands a comprehensive understanding for effective management. Recognizing the symptoms early, undergoing accurate diagnostic procedures, and following appropriate treatment modalities are vital to ensuring a favorable outcome. Equally important are preventive measures, including vaccination and hygiene practices, which play a crucial role in reducing the risk of pneumonia. By staying informed and taking proactive steps, individuals can safeguard their respiratory health and contribute to the overall well-being of the community.
References
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7241411/
https://www.nhlbi.nih.gov/health/pneumonia/
https://www.hopkinsmedicine.org/health/conditions-and-diseases/pneumonia
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7112285/
Was this article helpful?
YesNo




