Allergy
Blood Diseases
Bone & Joints
Brain
Cancer
Child Care
Cosmetic Surgery
Diabetes
Endocrinology
ENT
Eye
Gen Medicine
General Surgery
Heart
Kidney
Lifestyle
Liver & Digestive
Lung
Men’s Health
Mental health
Physiotherapy
Rheumatology
Skin and hair
Sleep Disorders
Spine
Transplant
Women Health
Thyroid
Vascular Surgery
Piles
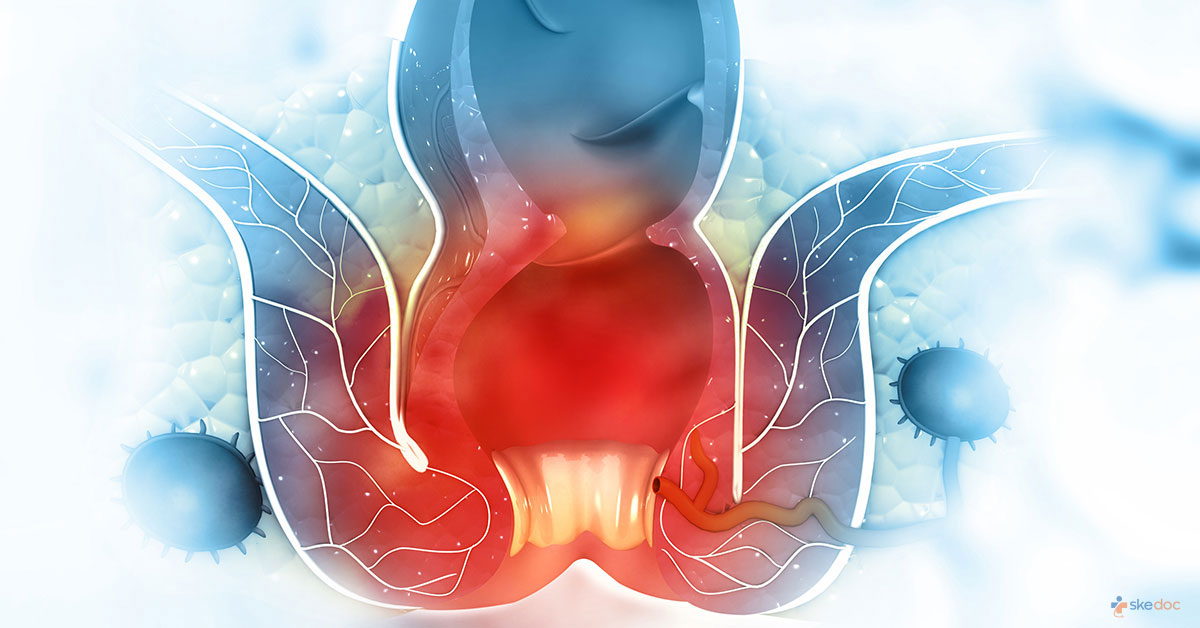
What are Piles?
Piles or Hemorrhoids is a condition in which the venous cushions in the lower part of the anal canal are swollen and inflamed. They can be either internal and remain inside the rectum or external and seen around the anus. They are among the most common conditions affecting the rectum and the anal canal.
Is Piles condition a Medical emergency?
Piles is not a medical emergency. However, if excessive bleeding does not stop, discharge, mass around the anus, painful defecation, or associated dizziness, it is advisable to seek medical attention.
Types
Types of Piles can be either:
- Internal Hemorrhoids: Lie within the rectum
- External Hemorrhoids: Present under the skin around the anus
- Interno-External Hemorrhoids
- Thrombosed Hemorrhoids: When there is pooling and clotting of the blood inside external Hemorrhoids
Causes
The exact cause of haemorrhoids is not fully understood. The venous cushions are important in protecting the internal and external anal sphincters and partly in preventing incontinence. They are made up of blood vessels called sinusoids, smooth muscle, and elastic connective tissue that becomes swollen and inflamed when either the venous pressure or the sphincter pressure increases.
Some of the causes for the development of haemorrhoids are:
- Straining during defecation
- Irregular bowel habits, constipation, diarrhea
- Sitting for an extended period on the toilet bowl
- The diet is low in fiber
- Obesity
- Pregnancy
- Aging
- Lack of exercise and a sedentary lifestyle
- Increased pressure inside the abdomen due to intra-abdominal masses or ascites
- Anal sex
Risk factors
The risk factors for developing Hemorrhoids include:
- Aging
- Pregnancy
- Sedentary and unhealthy lifestyle
- Higher socioeconomic status
- Lack of erect posture
- Liver disease
- Inflammatory bowel disease
- Spinal cord injury
- Anal sex
Symptoms & signs
Depending on the type of hemorrhoids, the symptoms may be:
- External Hemorrhoids:
- Itching or discomfort in the region around the anus
- Swelling around the anus
- Pain
- Bleeding
- Internal Hemorrhoids:
- Painless bleeding while passing stool
- If the Hemorrhoids protrude through the anus, they can cause pain, discomfort, and itching.
- Thrombosed Hemorrhoids:
- A hard mass and swelling around the anus
- Severe pain
- Redness and inflammation
Investigations
Investigations for establishing a diagnosis of Piles are not usually required, but an inspection of the entire colon is advisable. The following may be done:
- Laboratory tests: CBP & ESR to rule out infection and anemia
- Digital rectal examination
- Anoscopy
- Proctoscopy
- Sigmoidoscopy/Colonoscopy: To rule out other conditions of the colon that can cause bleeding, including Malignancy or IBD
Diagnosis
The diagnosis of piles is established based on medical history and clinical evaluation.
Course & stages
Internal Piles can be graded as follows:
- Grade I - There are only prominent vessels with no prolapse (sliding)
- Grade II - Prolapse upon straining but return spontaneously to the original position
- Grade III - Prolapse upon straining, but needs to be reduced manually
- Grade IV - Prolapse is present and cannot be reduced even manually
Treatment options
Treatment of piles can include conservative therapy to provide relief from the symptoms, and interventional procedures or surgery may be required in severe cases.
Medical management
Medical management of Hemorrhoids includes:
- Topical steroid creams: To reduce inflammation. It is only advisable to use it for up to 10 to 14 days.
- Oral analgesics: To provide relief from pain
- Stool softeners & Bulking Agents
- Topical anesthetics
- Mild astringent: To relieve itching
Interventions including surgery and indications for surgery
Non-surgical interventional procedures for the management of Piles should not be done in the presence of the following:
- HIV infected or immunocompromised individuals.
- Bleeding or clotting disorders
- Irritable bowel disease
- Rectal wall prolapse
- During pregnancy and immediately after delivery
- Anal fissure or infection
- If tumors are present
The interventional procedures include:
- Rubber band ligation: Suitable for grade II & III Piles. Done by placing one or two rubber bands to cut off the blood flow to the hemorrhoid so that it withers and falls off
- Coagulation, Electrocautery, and Electrotherapy: Suitable for grades I, II, and some grade III Piles. There are fewer complications than rubber band ligation. Done using either bipolar current or low voltage direct current
- Sclerotherapy and Cryotherapy: Usually done for grades I & II. Greater risk of complications and recurrence
- Radioablation: Useful in the management of recurrent Hemorrhoids.
- Laser therapy: Advanced method, similar effects as other methods with less recurrence rates but comparatively expensive
Surgical interventions for managing piles are only recommended if they are causing problems for the individual. Mildly symptomatic hemorrhoids are managed conservatively or with nonsurgical interventions.
The surgical intervention is indicated in the following conditions:
- Conservative or non-surgical interventions have failed to provide relief from bleeding, etc.
- Grade III & IV with severe symptoms
- Presence of other conditions of the anorectal canal that require surgical management
- It is preferred by the patient
The surgical procedures include:
- Surgical Hemorrhoidectomy - Laser or Scalpel or Harmonic
- Stapled Hemorrhoid surgery/procedure for prolapsing Hemorrhoids (PPH)/Minimally Invasive procedure for Hemorrhoids (MIPH)
- Doppler-guided transanal Hemorrhoidal dearterialization/Doppler Guided Hemorrhoidal Artery Ligation (DGHAL)
- Hemorrhoid artery ligation (HAL) with rectoanal repair (RAR)
Role of diet/ Exercise/ Lifestyle changes/ Preventive measures
Some measures that can be taken for relief from symptoms include:
- Eating a high fiber diet: To soften the stool and prevent straining
- Sitz bath 2 to 3 times a day: For relief from pain, itching and swelling
Some measures to prevent the formation of Hemorrhoids include:
- Eating a high fiber diet and taking fiber supplements
- Avoiding straining while passing stool
- Drinking lots of fluids
- Avoiding sitting for long periods, especially on the toilet bowl
- Passing stool as soon as the urge is felt without delaying for too long
- Getting regular exercise
Complications
- The complications of Piles include:
- Formation of blood clots
- Secondary infection
- Ulceration
- Incontinence
- Abscess formation
- Strangulation
- Complications of surgical procedures may include:
- Stenosis
- Infections
- Bleeding
- Non-healing wounds
- Formation of fistula
- Urinary retention
Prognosis
The prognosis for piles is generally good, and most cases resolve spontaneously or with conservative management. There is a higher chance of recurrence in managed conservatively or non-surgically circumstances when compared to surgically managed cases. Surgical complications occur in less than 5% of the cases.
When to contact the doctor or hospital? / How to identify the emergency or complications?
It is advisable to seek medical advice if there is excessive bleeding, and/or dizziness, or fainting.
Indications for hospitalization if required
Hospitalization may be needed if surgical intervention is required for the management of piles.
Suggested clinical specialist/ Departments to consult for this condition
The surgery departments will attend piles or haemorrhoids or colon and rectal surgery.
Was this article helpful?
YesNo
Comments





