Allergy
Blood Diseases
Bone & Joints
Brain
Cancer
Child Care
Cosmetic Surgery
Diabetes
Endocrinology
ENT
Eye
Gen Medicine
General Surgery
Heart
Kidney
Lifestyle
Liver & Digestive
Lung
Men’s Health
Mental health
Physiotherapy
Rheumatology
Skin and hair
Sleep Disorders
Spine
Transplant
Women Health
Thyroid
Vascular Surgery
Ulcerative colitis
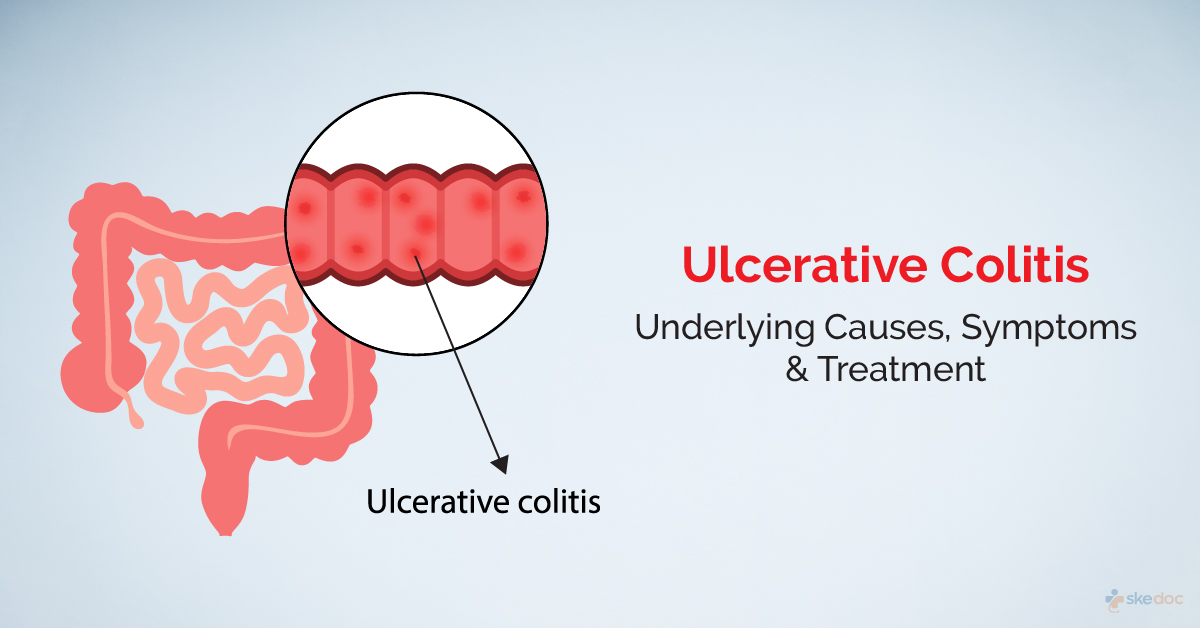
What is Ulcerative Colitis?
Ulcerative Colitis is a disease of the large intestine. It manifests as inflammation and ulceration of the colon and the rectum.
Is Ulcerative Colitis a Medical Emergency?
It has a diffuse spectrum of manifestations, of which bleeding per rectum is most common. Sometimes they present with low blood levels and persistent pain in the abdomen. It surely needs evaluation on an urgent basis.
Types
Depending on the location of the inflammation and ulceration may be of the following types:
- Ulcerative proctitis: It involves only the rectum
- Proctosigmoiditis: The rectum and the sigmoid colon are involved
- Left-sided Colitis: The rectum, sigmoid colon, and descending colon are affected
- Pancolitis: It affects the entire colon and the rectum
- Acute severe Ulcerative Colitis: It affects the entire colon and is the most severe form of the disease. Patients can have toxic megacolon, which can lead to bowel perforation too
Causes
The exact cause is unknown, but genetic causes, immune dysfunction, and environmental and lifestyle factors are implicated in its development.
Risk factors
The following may increase the risk of ulcerative colitis:
- Genetic susceptibility
- Family history or other inflammatory bowel diseases
- Psychological and psychosocial stress
- Excessive use of NSAIDs/ antibiotics abuse in childhood
Signs & Symptoms
The following symptoms and signs are seen
- Frequent stools
- Rectal bleeding
- Blood or mucus from the rectum
- Cramping rectal pain with a frequent urge to have a bowel movement (tenesmus)
- Lower abdominal pain
- Purulent discharge from the rectum (in the elderly)
- Weight loss
In fulminant (severe) Ulcerative Colitis, the symptoms may include:
- Severe diarrhea with cramps
- Fever
- Abdominal bloating, swelling and severe pain
- Tender abdomen
Investigations
The following investigations help establish a diagnosis:
- Laboratory tests:
- Serological markers: Such as Anti Neutrophil Cytoplasmic Antibodies (ANCA) and Anti Saccharomyces Cerevisiae Antibodies (ASCA)
- CBP & ESR
- C-Reactive Protein
- Other Inflammatory markers: Fecal Calprotectin, Fecal Lactoferrin, Alpha 1 antitrypsin
- Stool Examination
- Endoscopy & Biopsy: Flexible sigmoidoscopy/colonoscopy with multiple biopsy samples
- Imaging tests: sometimes CT/USG may show bowel thickening and oedema
Diagnosis
A diagnosis is established based on medical history, clinical evaluation, and investigations.
Treatment options
The treatment of this disease depends on the stage (whether it is active or in remission), the location, and the grade of the disease. The doctor may do initial medical management, followed by surgical intervention to treat and manage if required.
Medical management
Medical management is done to reduce the symptoms and prevent complications. This may include the following:
- Corticosteroids: It acts by reducing the inflammation; they are used in the initial management of moderate to severe ulcerative colitis
- 5 Aminosalicylic acid derivative: To reduce inflammation
- Immunosuppressant agents: To suppress the immune system and hence reduce the inflammation
Interventional including surgery and indications for surgery
Surgical management of this disease is indicated under emergencies such as Toxic megacolon, severe fulminant colitis, bowel perforation or when malignant transformation is considered. More electively considered when the disease is resistant to all medications or if there is intolerance. In such conditions, elective surgery may be considered.
Prognosis
The prognosis is generally good, and individuals with the disease have periods of activity followed by periods of remission. Improperly managed can result in morbidity and reduced quality of life, and there is a risk of developing colon cancer.
When to contact the doctor or hospital? / How to identify the emergency or complications?
It is advisable to seek medical attention if the symptoms are noticed.
Is regular screening indicated?
Individuals should get regular screening for colorectal cancer through colonoscopy as the risk increases with the duration of the disease.
Suggested clinical specialist/ Departments to consult for this condition
It will be attended by specialists from the Department's medical gastroenterology for diagnosis and further management.
Was this article helpful?
YesNo




