Allergy
Blood Diseases
Bone & Joints
Brain
Cancer
Child Care
Cosmetic Surgery
Diabetes
Endocrinology
ENT
Eye
Gen Medicine
General Surgery
Heart
Kidney
Lifestyle
Liver & Digestive
Lung
Men’s Health
Mental health
Physiotherapy
Rheumatology
Skin and hair
Sleep Disorders
Spine
Transplant
Women Health
Thyroid
Vascular Surgery
Systemic Lupus Erythematosus
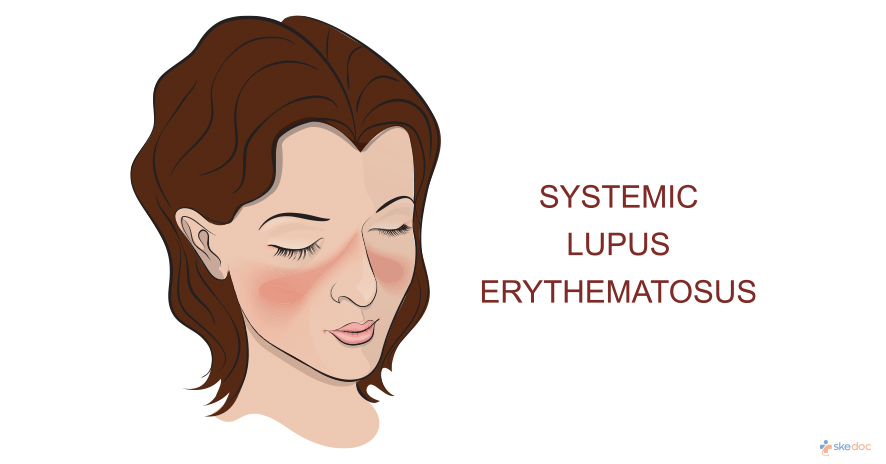
What is Systemic Lupus Erythematosus (SLE)?
Systemic Lupus Erythematosus (SLE), also known as Lupus, is a chronic autoimmune disorder in which the body’s immune system attacks its organs. The immune system of one’s body attacks its healthy tissue causing widespread tissue damage and inflammation. Systemic Lupus Erythematosus can affect the skin, joints, kidneys, brain, and various other organs. It is the most common type of lupus. It can range from mild to life-threatening conditions. It occurs in all age groups including children; however, it mostly occurs in women in the adolescent and postmenopausal age group.
Is Systemic Lupus Erythematosus a Medical emergency?
Systemic Lupus Erythematosus is not a medical emergency and is a long-term disorder.
Causes
The primary cause of Systemic Lupus Erythematosus is genetic mutations. Other factors include environmental triggers, such as exposure to ultraviolet rays, being on certain medications, viruses, trauma, or stress, exposure to chemical and pollutants can also result in the development of SLE. It affects more women when compared to men and it is believed that hormonal changes also play a role in the development of the condition.
Risk factors
A positive family history of Systemic Lupus Erythematosus in at least one first degree relative such as parents or siblings increases the risk of developing the disorder. Hormonal changes and being on certain medications can also increase the risk of developing the condition.
Symptoms & signs
Individuals having Systemic Lupus Erythematosus may sometimes have worsening episodes and sometimes have mild episodes. Symptoms change with time. Some of the signs and symptoms that an individual experiences include the following.
- Severe fatigue
- Headaches
- Arthritis, joint pain, and swelling
- Butterfly rash, especially on the cheeks and nose
- Hair loss
- Blood clotting problems
- Anemia
- Raynaud’s phenomenon (poor circulation to the fingers and toes with cold exposure)
- Sun sensitivity
- Oral ulcers
- Seizures
- Psychosis
- Immunological problems
- Lung, heart, and kidney problems
- Appetite loss
In some individuals, symptoms flare up and sometimes go away. Therefore, individuals have periods of flare-ups as well as remissions.
Investigations
A thorough physical examination of the body is done to identify the symptoms related to Systemic Lupus Erythematosus:
- Sun sensitivity rashes such as butterfly rash
- Ulcers on the inner layers of the mouth and nose
- Swelling or tenderness of joints of hands, feet, knees, and wrists
- Hair thinning and hair loss
- Any cardiac abnormalities such as irregular heartbeats or murmurs
Other diagnostic studies include the following:
- Complete blood count
- Antibody tests
- Urinalysis
- Chest x-ray
Diagnosis
It is difficult to diagnose because symptoms resemble many other conditions. Therefore, findings on a thorough physical examination along with results of the investigation tests are considered while establishing a diagnosis of Systemic Lupus Erythematosus.
Treatment options
Medical treatment
There is no treatment for Systemic Lupus Erythematosus. Treatment only focuses on controlling symptoms. The goal of the treatment of the condition is to prevent organ damage and achieve complete remission.
Medical treatment includes:
- Anti-inflammatory medications are prescribed to help with joint pain and stiffness. These drugs also help to reduce inflammation
- Steroid ointments for skin rashes
- Corticosteroids to minimize the immune response
- Antimalarial drugs for skin and joint problems
- Targeted immune system agents
- Immunosuppressants
Role of diet/ Exercise/ Lifestyle changes/ Preventive measures
Since the exact cause of the condition is not known, it cannot be prevented. Patient education, physical and lifestyle measures play a vital role in Systemic Lupus Erythematosus management. The following measures can help to lead a better life by controlling the symptoms.
Consume a healthy diet:
- Minimize stress levels by following stress reduction techniques
- Good sleep hygiene
- Physical exercises
- Smoking cessation. Smoking worsens Systemic Lupus Erythematosus symptoms
- Appropriate skincare is essential for curing skin rash as well as avoiding the further breakdown of the skin
- Aerobic exercises can help to decrease fatigue levels, which can including walking, swimming, and cycling
- Physical therapy to protect joints from getting damaged
Complications
It causes damage to all systems in the body. Some of the complications that are associated with this condition include:
- Inflammation of the heart
- Heart attack
- Stroke
- Blood clots and inflammation of blood vessels
- Memory changes
- Behavioural changes
- Inflammation of the lungs, kidneys, kidney dysfunction, and kidney failure
- Pregnancy complications including miscarriage
- Osteoporosis
- Limited physical and mental functioning
- Extreme fatigue
- Pregnancy complications
Prognosis
Most of the individuals with Systemic Lupus Erythematosus live a normal life with treatment. The prognosis varies from person to person. The overall outcome of the disease is highly variable ranging from permanent remission to death. In recent times, the survival rate of individuals suffering from SLE has increased from 5 years to 10 years.
When to contact the doctor? / How to identify complications?
Treatment of Systemic Lupus Erythematosus is effective when it is started in the early stages of the disease. Therefore, it is always recommended to consult a physician after noticing any of the symptoms associated with the condition.
Indications for hospitalization
Treatment is provided on an outpatient basis and does not require any hospitalization.
Suggested clinical specialists/ Departments to consult for this condition
Rheumatology.
Was this article helpful?
YesNo




