Allergy
Blood Diseases
Bone & Joints
Brain
Cancer
Child Care
Cosmetic Surgery
Diabetes
Endocrinology
ENT
Eye
Gen Medicine
General Surgery
Heart
Kidney
Lifestyle
Liver & Digestive
Lung
Men’s Health
Mental health
Physiotherapy
Rheumatology
Skin and hair
Sleep Disorders
Spine
Transplant
Women Health
Thyroid
Vascular Surgery
Glaucoma
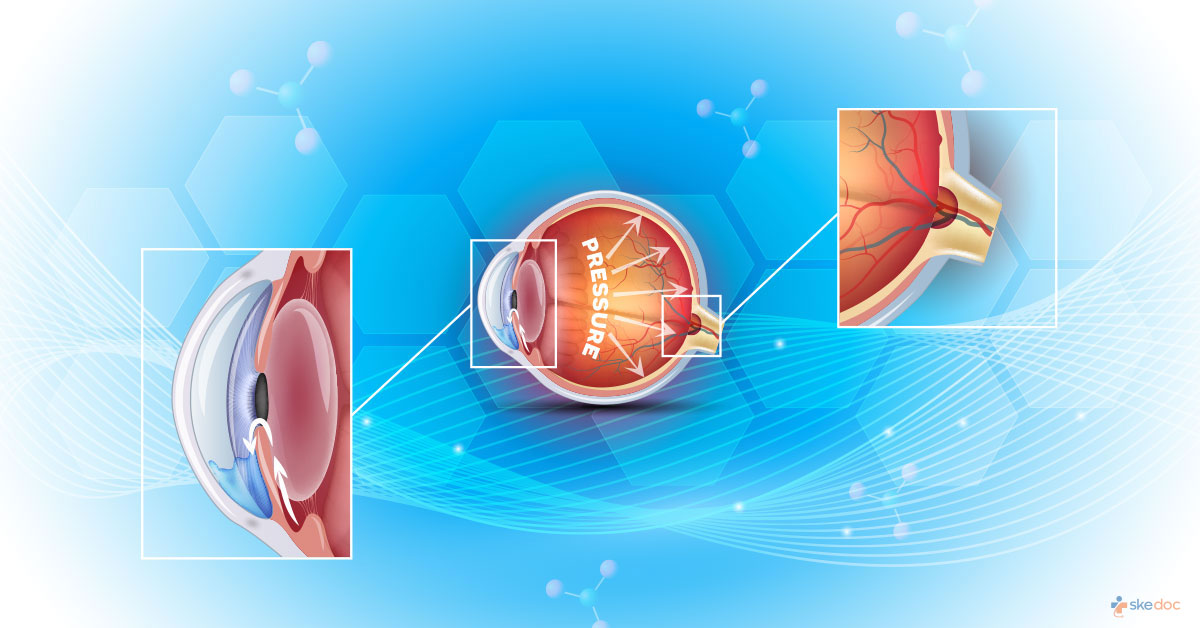
What is Glaucoma?
Glaucoma is a broad term describing conditions that lead to the damage of the optic nerve and loss of vision. The development of high pressure within the eye due to improper drainage of fluids is the most common cause of blindness.
Is Glaucoma a Medical emergency?
Glaucoma despite being a condition that develops slowly over time is a medical emergency and requires prompt medical attention to prevent loss of vision.
Types
Glaucoma can be of the following types:
- Primary Open-angle or Primary or Chronic Glaucoma is characterized by the slow clogging of the trabecular meshwork and increased intraocular pressure.
- High-tension
- Low-tension Glaucoma.
- Primary Narrow-angle Glaucoma is characterized by a narrowing of the angle where the eye drains, leading to increased intraocular pressure.
- Primary Angle-closure or Acute Glaucoma - The iris is in contact with the trabecular meshwork, closing the draining angle of the eye, and increasing the intraocular pressure.
- Acute Angle-closure Glaucoma (AACG)
- Chronic Angle-closure Glaucoma
- Intermittent Angle-closure Glaucoma
- Superimposed on Chronic open-angle closure Glaucoma
- Normal-tension or NTG or low tension or normal pressure Glaucoma of the optic nerve is damaged even though the intraocular pressure is normal.
- Pseudoexfoliation or PEX or Exfoliation Glaucoma is due to the presence of microscopic protein fibers that block the drainage and raise the intraocular pressure.
- Pigmentary Glaucoma or pigmentary dispersion syndrome is due to the accumulation of pigment cells that have sloughed off from the iris, blocking the trabecular meshwork, and raising the intraocular pressure.
- Primary Juvenile Glaucoma is seen in the newborn and is due to a developmental abnormality of the eye, with high intraocular tension at birth.
- Uveitic Glaucoma is seen in inflammation of the middle chamber of the eye (uveitis) and the intraocular pressure is raised either due to the inflammation of the corticosteroids that are used to treat it.
- Secondary Glaucoma develops as a result of another disease, condition, or drugs. It can be either an Open-angle or Closed-angle Glaucoma.
Causes
The cause of Glaucoma in most cases is the increase in the intraocular pressure within the eye. Any condition that obstructs the proper draining or the excess production of aqueous humor can lead to increased pressure. This in turn results in damage to the optic nerve and loss of vision.
Some of the causes may include:
- High blood pressure
- Diabetes
- Heart disease
- Sickle cell anemia
- High myopia (nearsighted) or high hypermetropia (farsighted)
- Uveitis
- Mature cataract
- Rupture of the lens capsule
- Subluxation (slipping) of the lens
- Intraocular hemorrhage (bleeding within the eye)
- Trauma
- After surgical interventions
- Drugs - corticosteroids, alpha chymotrypsin
- Intraocular tumors
- Retinal detachment
- Chemical burns
Risk factors
The risk factors for Glaucoma include:
- Age - Individuals over the age of 60 years are more at risk.
- Genetics - A family history of Glaucoma poses an increased risk.
- Race - Asian, African population is at a greater risk.
- Chronic medical conditions - Diabetes, Hypertension, Heart disease, Sickle cell anemia, etc.
- Eye trauma
- Thin cornea
- Medications - Extended use of corticosteroid eye drops.
- Being highly myopic (nearsighted) or hypermetropic (farsighted)
Signs & symptoms
The symptoms and signs of Glaucoma include:
- Severe headaches
- Pain in the eyes
- Blurred vision
- Halos around lights
- Redness of eyes
- Blind spots in the central or side vision
- Tunnel or tubular vision
Investigations
The investigations that are done to establish a diagnosis of Glaucoma include:
- Tonometry - To measure the pressure inside the eye
- Ophthalmoscopy - To check the shape and color of the optic nerve
- Perimetry - To check the entire field of vision
- Gonioscopy - To evaluate the angle of the eye where the iris meets the cornea, and where the draining of the aqueous humor occurs
- Pachymetry - To measure the thickness of the cornea
- Nerve fiber analysis - To measure the thickness of the optic nerve fiber layer
Diagnosis
Diagnosis of Glaucoma is arrived at based on medical history, clinical evaluation, and the results of the investigations.
Course & Stages
It is a slow-progressing disease and the following stages occur in the progress of the disease:
- Stage 1: The initial sequence of events that leads to stage 2
- Stage 2: Alteration in the aqueous humor drainage system
- Stage 3: Elevated intraocular pressure
- Stage 4: Optic nerve damage
- Stage 5: Complete loss of vision
Treatment options
The damage and vision loss cannot be reversed, but early diagnosis and treatment can help to slow the progression of the condition and prevent further damage and complete vision loss.
Medical management
Medical management of Glaucoma includes eyedrops such as:
- Prostaglandins: To increase the outflow of the aqueous humor
- Beta-blockers: To reduce fluid production in the eye
- Alpha-adrenergic stimulants: To reduce production and increase the outflow of the fluids in the eye
- Carbonic anhydrase inhibitors: To reduce fluid production in the eye
- Rho-kinase inhibitors: To reduce the fluid production and decrease the intraocular pressure
- Miotic agents: To increase the outflow of fluid from the eye
Oral medication may be prescribed if eye drops are not effective and include oral doses of carbonic anhydrase inhibitors.
Interventional including surgery and indications for surgery
Surgical intervention may be required in quite a few cases to reduce the intraocular pressure and the procedures include:
- Laser trabeculoplasty:
- Argon laser trabeculoplasty (ALT) - It is a temporary solution to treat open-angle Glaucoma.
- Selective laser trabeculoplasty (SLT) - Selectively targets the melanocytes in the trabecular meshwork, and is a long term treatment.
- Iridotomy
- Laser peripheral iridotomy (LPI) - Done to decrease the intraocular pressure by making small openings in the iris and removing very small amounts of iris tissue.
- Iridectomy or corectomy or surgical iridectomy: Involves the removal of small portions of the iris tissue to decrease intraocular pressure.
- Trabeculectomy: It is the most commonly done procedure in which a small portion of the trabecular meshwork is removed to help in the drainage of the fluid from the eye.
- Laser-assisted non-penetrating deep sclerectomy (NDPS): A modified trabeculectomy with lesser side effects.
- Canaloplasty: It is a minimally invasive procedure done using a microcatheter to help with the drainage of fluid from the eye.
- Glaucoma drainage implants: Its valves or tubes are placed within the trabecular meshwork to help with the drainage of fluids.
- Ciliary destructive: This is done to destroy some cells in the ciliary body that produce aqueous humor, thereby reducing the intraocular pressure.
Role of diet/ Exercise/ Lifestyle changes/ Preventive measures
Some measure that can be taken to prevent and from developing or from worsening includes:
- Getting regular eye examinations - Especially if there is a family history, or if there are other health conditions that predispose to diseases such as diabetes, high blood pressure, heart disease, etc.
- Eating a healthy diet - Especially with foods rich in zinc, selenium, Vitamins A, C, & E.
- Regular exercise
- Moderating the consumption of coffee.
- Sleeping with the head elevated.
- Avoiding drinking a lot of fluids in one go.
- Taking medications prescribed for the prevention or treatment of disease regularly and in the prescribed dose.
Complications
Permanent loss of vision is the most serious complication of Glaucoma.
Prognosis
When the prognosis is detected and treated early is good, especially for open-angle Glaucoma.
When to contact the doctor or hospital? / How to identify the emergency or complications?
It is advisable to seek medical attention immediately if there are any symptoms of Glaucoma, especially such as tunnel vision, blurring of vision with headaches, or halos around lights.
Indications for hospitalization if required
Hospitalization is usually not required but may be required for surgical management.
Suggested clinical specialist/ Departments to consult for this condition
Glaucoma is attended to by specialists and ophthalmologists.
Additional Information
It is the second leading cause of blindness worldwide.
Was this article helpful?
YesNo




