Allergy
Blood Diseases
Bone & Joints
Brain
Cancer
Child Care
Cosmetic Surgery
Diabetes
Endocrinology
ENT
Eye
Gen Medicine
General Surgery
Heart
Kidney
Lifestyle
Liver & Digestive
Lung
Men’s Health
Mental health
Physiotherapy
Rheumatology
Skin and hair
Sleep Disorders
Spine
Transplant
Women Health
Thyroid
Vascular Surgery
Dyslipidemia
What is Dyslipidemia?
Dyslipidemia is the presence of abnormal levels or imbalance of lipids commonly known as fats such as cholesterol, triglycerides, low-density lipoproteins (LDL), and high-density lipoproteins (HDL) in the body. Lipids are absorbed through the intestine and are essential for the production of energy, steroids, and bile acid.
Is Dyslipidemia a Medical emergency?
Dyslipidemia is not a medical emergency, but over time uncontrolled Dyslipidemia can result in medical conditions that can precipitate as medical emergencies.
Types
Dyslipidemia may be classified as follows:
- Primary Dyslipidemia – due to genetic factors
- Secondary Dyslipidemia – caused due to lifestyle and other factors
Dyslipidemia may also be of the following types:
- Hyperlipidemia – the increased presence of lipids
- Hypercholesterolemia – increased cholesterol
- Hyperglyceridemia – increased glycerides
- Hypertriglyceridemia – increased triglycerides
- Hyperlipoproteinemia – increased LDL lipoproteins
- Combined Hyperlipidemia – both LDL and triglycerides are increased
- Hypolipidemia – low levels of lipids
- Hypocholesterolemia – low levels of cholesterol
- Hypolipoproteinemia – low levels of lipoproteins
- Abetalipoproteinemia – low levels of beta lipoproteins
- Tangier’s Disease – low levels of HDL
Causes
Several factors including genetic, environmental, and lifestyle can contribute to an imbalance in the levels of lipids in the body. Some of them include:
- Genetic factors:
- Autosomal dominant genetic mutations in the LDL receptors and pathways
- Autosomal dominant genetic mutations in the cholesterol pathway
- Lifestyle and environmental factors:
- Smoking
- Physical inactivity
- Improper nutrition with excessive intake of calories
- Obesity
- Improper consumption of vegetables, fruits, nuts, and seeds
- High consumption of saturated fatty acids, trans fats,
- Alcohol overuse
- Medications – such as beta-blockers, thiazide diuretics, corticosteroids, antiretroviral agents, retinoids, estrogen, and progestin supplementation
- Medical conditions:
- Diabetes
- Chronic kidney disease
- Hypothyroidism
- Liver diseases
Risk factors
Factors that increase the risk of Dyslipidemia include:
- Family history of atherosclerotic disease
- Diabetes
- Chronic kidney disease
- Smoking and alcohol overuse
- Sedentary lifestyle
- Unhealthy food habits
Symptoms & Signs
The signs and symptoms of Dyslipidemia manifest as an asymptomatic disease of the vascular system and may include the following:
- Presence of yellowish fat deposits visible on the skin of the eyelids, palms, and tendons; they can turn into plaques or nodules
- Joint pains
- Enlargement of the liver
- Enlargement of the spleen
- Numbness and abnormal sensation in the hands and feet
- Stroke
- Coronary artery disease
- Chest pain, breathlessness, etc.
- Peripheral arterial disease
- Pain when walking, or rest pain in severe cases, ischemic ulcers, gangrene
Investigations
Some investigations that are advised for the evaluation of Dyslipidemia include:
- Laboratory tests:
- CBP & ESR
- Lipid Profile – fasting lipid profile done in adults and children with known risk factors
- Cholesterol
- Triglycerides
- LDL and VLDL
- HDL
- Blood Glucose
- Liver function tests
- Renal function tests
- Thyroid Profile
- Complete urine analysis
- ECG
Diagnosis
A diagnosis of Dyslipidemia is established based on medical history, clinical evaluation, and results of the investigations done.
Treatment options
The main aim of the treatment of Dyslipidemia is to prevent its progress to complications such as cardiovascular disease and stroke. The options for treatment depend on the type of Dyslipidemia and the severity of the condition. Mild and initial stages of the condition in the absence of significant risk factors do not require pharmacological therapy and can be managed with simple lifestyle modifications
Medical management
Medical management of Dyslipidemia may include the following:
- Statins – To lower cholesterol and LDL levels; they are prescribed when
- When there is clinical evidence of atherosclerotic cardiovascular disease
- When the cholesterol LDL is more than 190mg/dl
- When the age of the individual is between 40-75, with the presence of diabetes, and LDL cholesterol between 80-190mg/dl
- Bile Acid Sequestrants – Act by blocking bile acid reabsorption, thereby increasing the uptake of cholesterol for the formation of bile acid; they are usually used in combination with statins
- Cholesterol Absorption Inhibitors – such as ezetimibe; act by stopping the absorption of cholesterol in the intestines and help to lower LDL
- PCSK9 monoclonal antibodies – given as subcutaneous injections; help with the reduction of LDL levels
- Mipomersen gave as subcutaneous injections and lomitapide orally
- Fibrates – to lower triglycerides and increase HDL levels
- Omega 3 Fatty Acids – to lower triglycerides
- Apo CIII inhibitors – to lower triglycerides
- Nicotinic Acid – to elevate HDL levels
- CETP inhibitors – to raise HDL levels by stopping the action of cholesterol ester transport proteins
Interventional including surgery and indications for surgery
Procedures that may be done for the management of severe Dyslipidemia that is not responding to conventional management include:
- Apheresis – The LDL is removed with the help of extracorporeal plasma exchange
- Ileal bypass surgery – To block the reabsorption of bile acids
Role of diet/ Exercise/ Lifestyle changes/ Preventive measures
Some measures that can help with the management and prevention of Dyslipidemia include:
- Eating a healthy diet while monitoring calorie intake
- Maintaining an active lifestyle and an ideal body weight
- Participating in moderate to vigorous aerobic physical activity up to 40 minutes 3-4 times a week
- Avoiding smoking
- Avoiding alcohol overuse
- An eating diet rich in fiber and complex carbohydrates, with foods such as vegetables, fruits, nuts, and seeds
Complications
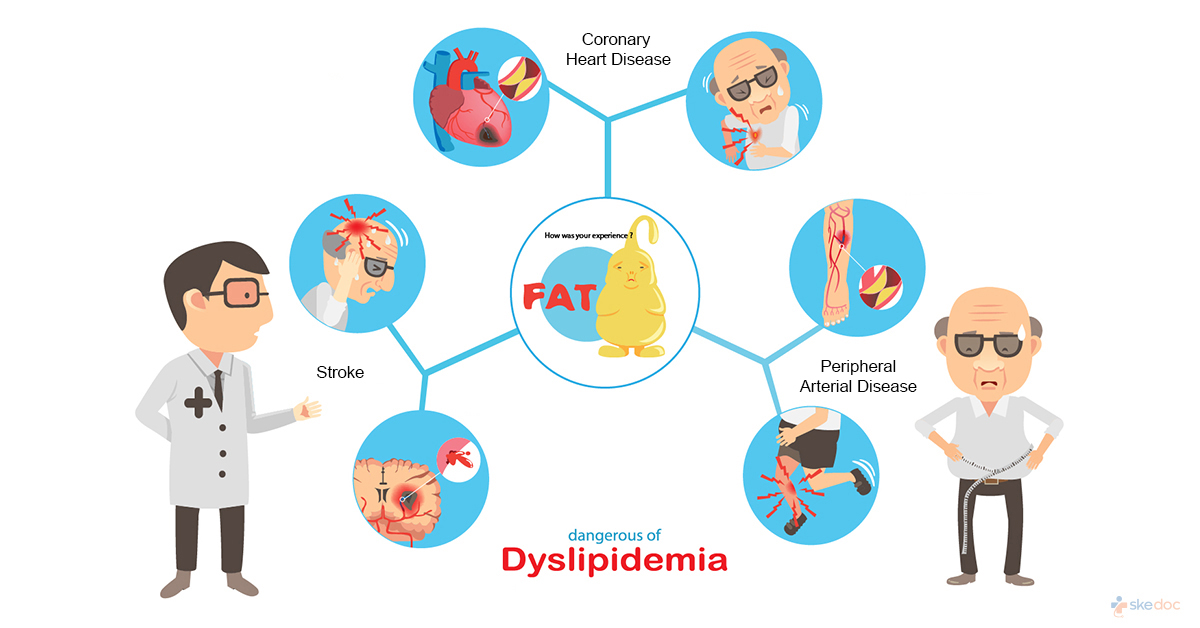
Some complications associated with Dyslipidemia include:
- Increased risk of heart disease
- Sudden cardiac death
- Acute myocardial infarction
- Peripheral arterial disease
- Transient ischemic attacks
- Stroke
- Death
Prognosis
The prognosis of Dyslipidemia depends on the type and severity of the condition and the presence of risk factors that increase the possibility of atherosclerotic cardiovascular disease. Early diagnosis and modification of lifestyle along with proper management decreases the likelihood of progression to complications.
When to contact the doctor or hospital? / How to identify the emergency or complications?
It is advisable to seek medical attention if the signs and symptoms of Dyslipidemia are noticed.
Indications for hospitalization if required
Hospitalization is not required for the management of Dyslipidemia unless major interventions are advised for the management of severe disease not responding to conservative therapy.
Screening methods
It is advisable for individuals with a family history of atherosclerotic cardiovascular disease, to monitor their lipid levels at regular intervals.
Suggested clinical specialist/ Department to consult for this condition
- Cardiology
Was this article helpful?
YesNo




