Allergy
Blood Diseases
Bone & Joints
Brain
Cancer
Child Care
Cosmetic Surgery
Diabetes
Endocrinology
ENT
Eye
Gen Medicine
General Surgery
Heart
Kidney
Lifestyle
Liver & Digestive
Lung
Men’s Health
Mental health
Physiotherapy
Rheumatology
Skin and hair
Sleep Disorders
Spine
Transplant
Women Health
Thyroid
Vascular Surgery
VSD in Kids
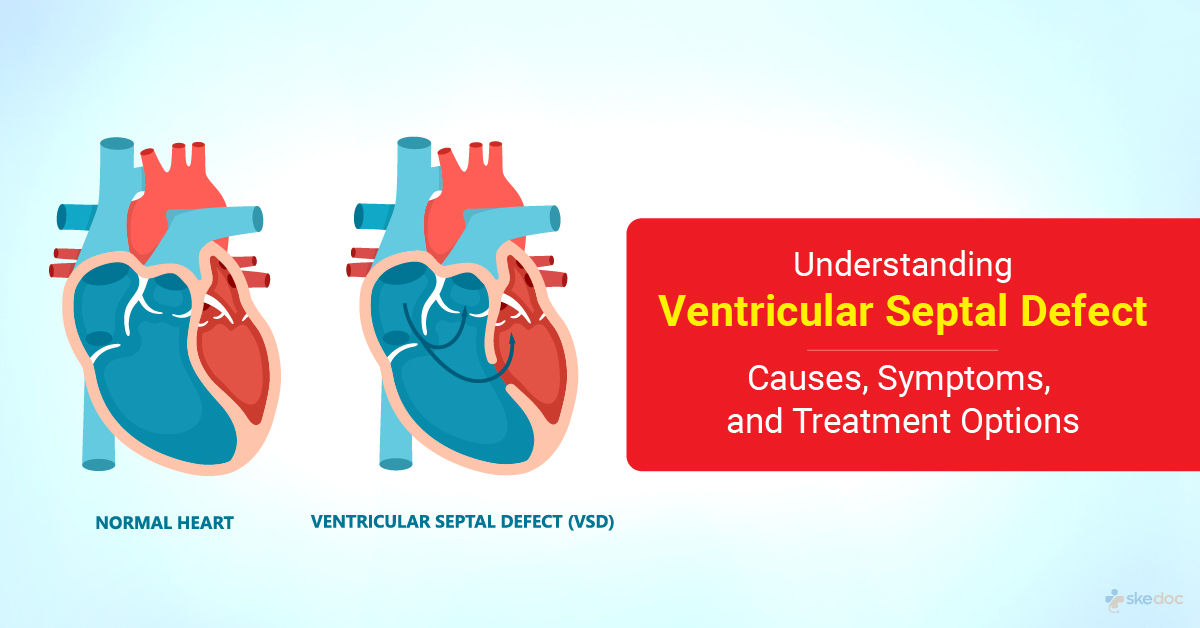
What Is Ventricular Septal Defect (VSD) In Kids?
Ventricular Septal Defect (VSD) in children is a birth defect in which an abnormal opening in the wall separates the heart's left and right lower chambers (ventricles). The defect may be a small opening or may be so large that it results in the presence of a single lower chamber. The wall between the two chambers has a lower muscular and an upper membranous portion, and the defect may be present in either one or both. Most of the defects are seen in the membranous portion of the septum. While most defects close independently, some require Ventricular Septal Defect (VSD) surgery.
Is this condition a medical emergency?
Ventricular Septal Defect in children is not a medical emergency.
Types of this condition
Ventricular Septal Defect (VSD) types in children may be as follows.
- Perimembranous Ventricular Septal Defect: The defect is near the left ventricle outflow tract just below the aortic valve.
- Supracristal Ventricular Septal Defect: The defect lies below the pulmonary valve and communicates with the right ventricle outflow tract.
- Muscular Ventricular Septal Defects: Are present entirely in the muscular portion of the septum and are usually multiple.
Causes of VSD in Children
The exact reason for forming Ventricular Septal Defects in children is not fully understood. However, some of the following factors may play a role.
- Genetic and Hereditary factors
- Environmental Factors
- Infections: Rubella
- Drugs: Lithium, alcohol, hydantoin, thalidomide
Risk Factors
Some risk factors for the development of Ventricular Septal Defects include
- Maternal diabetes, SLE, phenylketonuria
- Maternal obesity
- Maternal and paternal alcoholism
Symptoms & signs
The symptoms and signs associated are dependent on the size of the defect and may include
- Small Ventricular Septal Defect: No symptoms are usually seen in a Small Ventricular Septal Defect; feeding or weight gain is also not much affected in small Ventricular Septal Defects.
- Moderate Ventricular Septal Defect: Usually seen around the age of 2-3 months or in early infancy
- Excessive sweating during feeding
- Fatigue associated with feeding
- Rapid breathing at rest or with feeding
- Lack of growth
- Frequent respiratory infections
- Poor weight gain
- Mildly increased heart rate
- Enlarged liver
- Large Ventricular Septal Defect: The symptoms and signs are similar to Moderate Ventricular Septal Defect but are much more severe and may be seen earlier than at 2 months of age.
Investigations
The following investigations are usually done for the condition.
- Laboratory tests
- CBP & ESR
- Complete Metabolic Panel
- Coagulation profile and blood typing
- Arterial blood gas measurement
- Imaging tests
- Chest X-Ray
- 2 D Echocardiography
- Doppler Echocardiography and Color Flow Imaging
- MRI
Diagnosis
A diagnosis of VSD in children is established based on medical history, clinical evaluation, and investigation results.
Treatment
The treatment depends on the size of the defect and the severity of the condition. Children with small Ventricular Septal Defects do not require medical or surgical therapy. Children with moderate Ventricular Septal Defect may require medical therapy for the management of congestive heart failure. Surgical intervention is the ideal treatment of choice if any treatment is necessary, as most of these defects tend to close on their own.
Medical management
Medical management of congestive heart failure in children with Ventricular Septal Defect may include the following.
- Diuretics
- ACE inhibitors
- Inotropic agents
- High caloric density feeding
Interventional including surgery and indications for surgery
Surgical intervention is indicated in the following conditions.
- Large ventricular septal defects, which are asymptomatic, are often repaired between 6 and 12 months of age.
- Large Ventricular Septal Defects in older children even though they are asymptomatic if the pulmonary to systemic flow ratio is high.
- Moderate Ventricular Septal Defects with uncontrolled congestive heart failure, growth failure, and recurrent respiratory infections.
Surgical intervention may include
- Open Heart Surgery: For the management of membranous Ventricular Septal Defects, direct surgical repair using cardiopulmonary bypass is done. In infants with multiple Ventricular Septal Defects or those who are critically ill or have other cardiac defects, a Pulmonary Artery Banding is done as a 2 2-stage procedure. Ventricular Septal Defects present at the ventricular inlet or perimembranous defects are repaired by approaching them through the atria. If the defects are present in or near the outlet, they are approached through the pulmonary valve.
- Transcatheter/Minimally invasive surgery: To manage Muscular Ventricular Septal Defects – these surgeries are done under trans-esophageal echocardiography guidance. Ventricular septal defect closure may be done by using the Amplatzer membrane VSD occluder device, a self-expanding device used in older infants.
Role of Diet/Exercise/Lifestyle changes/ Preventive measures
Some measures that may be needed for the management of Ventricular Septal Defects in Children
- Periodic monitoring and cardiology consultations
- High-calorie diet in infants
- Antibiotic prophylaxis before undergoing surgical or dental procedures
- Good hand and oral hygiene to reduce the risk of infections
Complications
Some of the complications of VSD in children include
- Congestive heart failure
- Heart Arrhythmias
- Pulmonary hypertension
- Stroke
- Infective Endocarditis
- Pericardial effusion
- Sudden death
Prognosis
The prognosis of ventricular septal defects in children is excellent in the case of minor ventricular septal defects. The prognosis of Moderate Ventricular Septal Defects and Large Ventricular Septal Defects is also good if they are detected and managed early.
When to contact the doctor or hospital? / How to identify the emergency or complications?
It is advisable to seek medical attention if the symptoms and signs of Ventricular Septal Defects in children are noticed.
Indications for hospitalization if required
Hospitalization will be required for the surgical management of Ventricular Septal Defects in children.
Screening methods
Individuals who have undergone surgical procedures to treat Ventricular Septal Defects should be followed up to look for long-term complications of both surgical procedures and the condition itself. In children with membranous and perimembranous Ventricular Septal Defects, the risk of aortic valve leaflet prolapse and aortic insufficiency is high, in addition to the formation of the left ventricle to right atrium shunts.
Additional info
For pregnant women with un-operated Ventricular Septal Defects, which are mild and asymptomatic, the management of pregnancy and labor is done as it is done for pregnant women without a Ventricular Septal Defect. No antibiotic prophylaxis is required for these women. Women with Ventricular Septal Defects that are symptomatic are treated as a high-risk pregnancy and managed as such. In all these women, induced labor and vaginal delivery are preferred over cesarean section delivery. Cesarean section deliveries are associated with higher blood loss and more postoperative complications that women with Ventricular Septal Defects may not tolerate.
Suggested clinical specialist/Departments to consult for this condition
Specialists from the Department of Paediatric Cardiology, Congenital Heart Disease, will attend to Ventricular Septal Defects in children.
Was this article helpful?
YesNo




