Allergy
Blood Diseases
Bone & Joints
Brain
Cancer
Child Care
Cosmetic Surgery
Diabetes
Endocrinology
ENT
Eye
Gen Medicine
General Surgery
Heart
Kidney
Lifestyle
Liver & Digestive
Lung
Men’s Health
Mental health
Physiotherapy
Rheumatology
Skin and hair
Sleep Disorders
Spine
Transplant
Women Health
Thyroid
Vascular Surgery
TOF
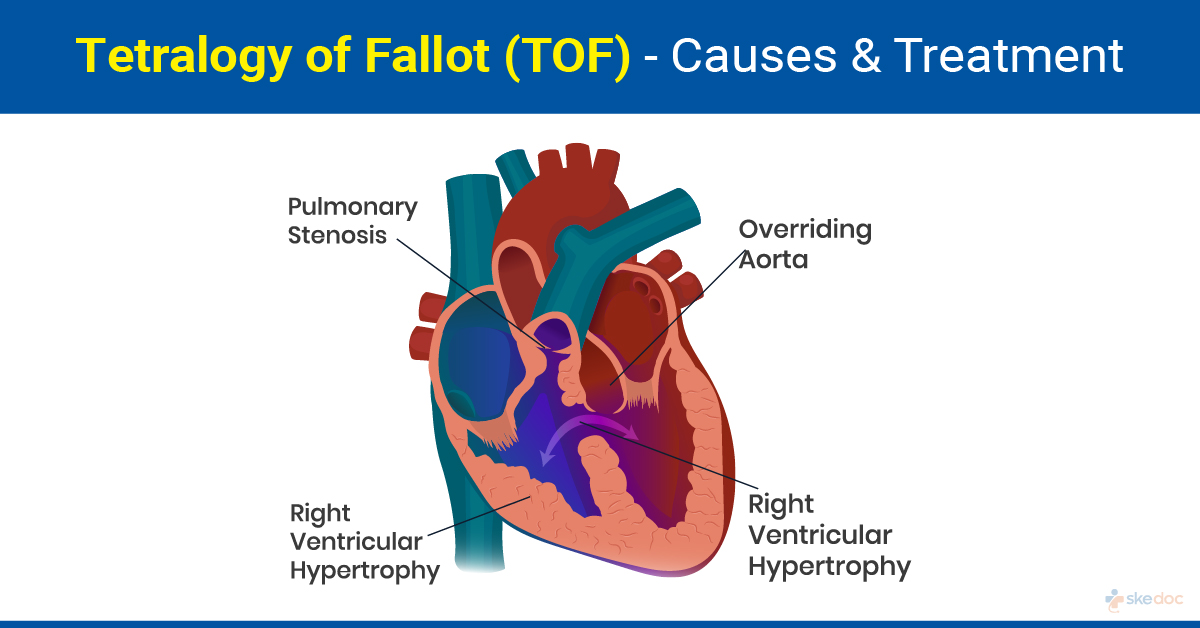
What is Tetralogy Of Fallot (TOF)?
Tetralogy of Fallot (TOF) is a birth defect that results in abnormal development of the heart with four major structural defects. It is classified as a cyanotic congenital heart defect as it results in an inadequate flow of blood to the lungs for oxygenation.
Is this condition a medical emergency?
Untreated tetralogy of fallot can lead to medical emergencies depending on its severity.
Causes
The exact cause is not fully understood, but the defect occurs during fetal development. Four major defects comprise TOF which include
- Pulmonary valve stenosis: The valve that regulates the flow of blood between the right lower chamber of the heart and the pulmonary artery that carries the blood to the lungs is narrowed.
- Ventricular septal defect: There is a hole in the wall that separates the two lower chambers of the heart, namely the left and the right ventricle, resulting in a mixing of the deoxygenated blood in the right chamber with the oxygenated blood in the left chamber.
- Overriding of the Aorta: The aorta, which normally arises out of the left ventricle and supplies blood to the body, is shifted slightly to the right and lies above the ventricular septal defect.
- Right ventricular hypertrophy: There is a thickening, stiffening, and enlargement of the muscle of the right ventricle.
In addition to the four main TOF components, the following may also be present
- Narrowing of the left pulmonary artery
- A bicuspid pulmonary valve
- Right-sided aortic arch
- Anomalies of the coronary arteries
- Atrial septal defect or a patent foramen ovale
- Atrioventricular septal defect
- Partial or total anomalous pulmonary venous return
- Pulmonary Atresia
Risk factors
Some of the risk factors that are associated with the development of Tetralogy of Fallot include
- Maternal Rubella or other viral infection during pregnancy
- Maternal alcoholism
- Maternal Phenylketonuria
- Maternal age of more than 40 years
- Maternal Diabetes
It is also seen to be associated with CATCH 22, which is cardiac defects, abnormal facies, thymic hypoplasia, cleft palate, hypocalcemia, and chromosome 22 abnormalities.
Symptoms & Signs
The symptoms and signs may show soon after birth or may present late in life, depending on the severity of the condition. Some of them include
- Symptoms in infants and children
- Difficulty feeding
- Failure to thrive
- Tet Spells: episodes of bluish skin and face while feeding or crying
- Breathlessness on exertion
- Squatting to compensate for breathlessness due to exertion
- Coughing up of blood
- Symptoms in Adults
- Lack of exercise endurance
- Palpitations
- A gradual decline in body functions
- Syncope
- Swelling of feet, ankles, and legs
- Swelling of the abdomen (ascites)
Cyanosis is worsened in TOF in infants and children if the following are additionally present
- Dehydration
- Stress
- Infections
- Exercise
Investigations
Some investigations that are done for establishing a diagnosis include
- Laboratory tests:
- CBP & ESR
- Coagulation Profile and Blood typing
- Liver and renal function tests
- Blood Cultures
- Arterial Blood Gas measurement
- Electrocardiography
- Cardiac Catheterization: It is usually done for suspected Tetralogy of Fallot in adults; it is done when the anatomy is not completely identified on echocardiography, or when there might be a disease in the pulmonary vessels, or if pulmonary hypertension is present or may develop. Cardiac catheterization is useful in the assessment of pulmonary valve size and the pulmonary arteries, the right ventricular outflow tract obstruction, the location, position, and size of the ventricular septal defect, and for ruling out another coronary artery disease.
- Imaging tests:
- Chest-X-Ray: Tetralogy of Fallot X-ray findings are described as a boot-shaped heart with decreased vascularity of the lungs and less prominent pulmonary arteries. Tetralogy of Fallot X-ray imaging is important in the newborn and infants to assess the blood flow to the lungs. Tetralogy of Fallot X-ray findings in children may show an enlarged aorta with a right-sided aortic arch. All these findings are important for planning the surgery for TOF.
- Echocardiography: It is currently the preferred imaging method for Tetralogy of Fallot in infants and children. 2D echocardiography is used for the assessment of intracardiac abnormalities. Doppler ultrasonography is useful in the measurement of the pressure gradient and blood flow in the Tetralogy of Fallot.
- MRI: Spin-Echo MRI is used to visualize the cardiac defects, including outflow obstruction, ventricular septal defect, overriding of the aorta, and right ventricular hypertrophy in Tetralogy of Fallot in children.
- Angiography: It is useful to visualize the vascular defects and blood flow in TOF, but in most cases, non-invasive methods such as echocardiography and MRI are preferred.
Diagnosis
A diagnosis of Tetralogy of Fallot is established based on medical history, clinical evaluation, and results of the investigations done.
Treatment options for Tetralogy of Fallot
Surgical interventions are the definitive treatment for Tetralogy of Fallot. Surgery for Tetralogy of Fallot in children is not a definitive treatment, and further primary and secondary surgical interventions may be required at different stages of life.
Medical management
Medical management of TOF is limited to reducing the ventilatory drive, increasing the peripheral vascular resistance, and increasing the venous return to the heart. It may include
- Analgesics
- Alpha Adrenergic Agonists: Improve the heart muscle contraction and heart rate, cause an increase in cardiac output, and increase the peripheral vascular resistance.
Interventional including surgery and indications for surgery
Interventional management of TOF includes the following surgical procedures
- Surgical intervention in infants: This is done to close the ventricular septal defect, reduce the pulmonary stenosis, and relieve the right ventricle outflow obstruction. Additional defects, such as an atrial septal defect or patent foramen ovale, are also closed.
- Surgical Intervention in adults: The ventricular septal defect is closed, the infundibulum is widened, and the pulmonary valve is repaired or replaced. If surgery was done in infancy, then a replacement of the pulmonary valve with a prosthetic valve is usually done.
Role of Diet/Exercise/Lifestyle changes/ Preventive
Some measures that may be needed in individuals with TOF who have had surgical interventions include
- Cardiac rehabilitation
- Regular and periodic cardiologic check-ups well into adult life
- Antibiotic prophylaxis before surgical or dental procedures
- Maintaining good hand and respiratory hygiene to avoid infections
Complications
Some complications that can be seen in individuals with TOF include
- Right heart failure
- Atrial and ventricular arrhythmias
- Endocarditis
- Septic central emboli
- Sudden death
Prognosis
The prognosis of TOF that is diagnosed, treated, and periodically followed up is generally good. Untreated TOF with severe defects has a high mortality. The prognosis of surgery for TOF in adults is poor in the following conditions
- Advanced age
- Poor right ventricular function
- Cardiogenic shock
- Multiple ventricular septal defects
- Diseased or small pulmonary arteries
- Coronary artery disease and disease of other valves
When to contact the doctor or hospital? / How to identify the emergency or complications?
It is advisable to seek medical attention if the symptoms and signs of TOF are noticed.
Indications for hospitalization if required
Hospitalization will be required for the treatment of TOF.
Suggested clinical specialist/departments to consult for this condition
TOF will be attended to by specialists from the Department of Cardiology, Paediatric Cardiology, and Adult Congenital Heart Disease.
Was this article helpful?
YesNo




