Allergy
Blood Diseases
Bone & Joints
Brain
Cancer
Child Care
Cosmetic Surgery
Diabetes
Endocrinology
ENT
Eye
Gen Medicine
General Surgery
Heart
Kidney
Lifestyle
Liver & Digestive
Lung
Men’s Health
Mental health
Physiotherapy
Rheumatology
Skin and hair
Sleep Disorders
Spine
Transplant
Women Health
Thyroid
Vascular Surgery
Endocarditis
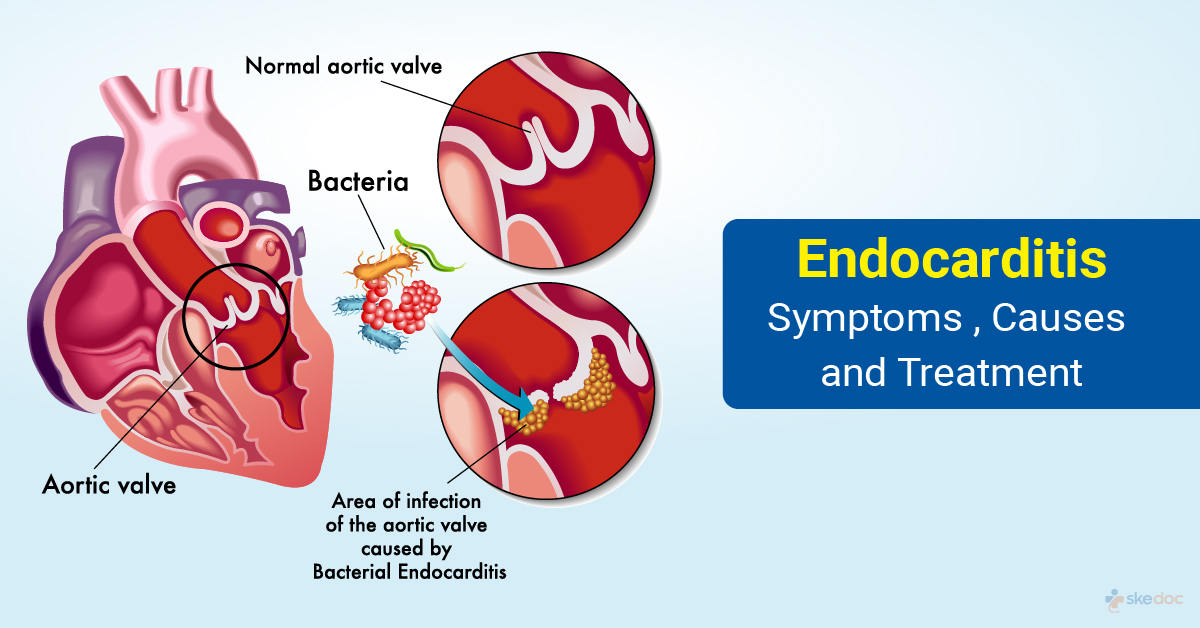
What is Endocarditis?
Endocarditis is an inflammation of the endocardium which is the innermost layer of tissue of the heart. The endocardium lies below the myocardium which is the muscular layer of the heart that aids in heart contractions. It can involve the heart valves, the interventricular septum, tendinous structures that are attached to the mitral and the tricuspid valves, and devices that are placed inside the heart.
Is this condition a medical emergency?
Endocarditis is not a medical emergency, but early medical attention is warranted to prevent serious complications.
Types of endocarditis
Endocarditis may be of the following types:
- Infective Endocarditis: Due to an infection of the endocardium with microorganisms.
- Native valve infection
- Acute native valve infection
- Sub-acute native valve infection
- Prosthetic valve infection
- Early prosthetic valve infection
- Late prosthetic valve infection
- Intravenous drug abuse endocarditis infection
- Nosocomial (hospital-acquired) infective endocarditis
- Pacemaker infective endocarditis
- Native valve infection
- Non-infective/non-bacterial thrombotic/Libman-sacks/verrucous or marantic endocarditis: Inflammation of the endocardium due to causes other than infections with microorganisms.
Causes
Endocarditis pathophysiology shows that infective inflammation of the heart valve mostly develops on the mitral valve, followed by the aortic, tricuspid, and finally the pulmonary valve in order of preference. This also shows that the conditions are brought initially by bacteremia that delivers the microorganisms to the valve, followed by the sticking of these organisms to the valves, and finally the invasion of the valve leaflets by these organisms.
The presence of sterile vegetation which is formed due to fibrin and platelet aggregation is an important factor in the development of infective inflammation of the heart valve. The sterile vegetation aids the bacteria or other microorganisms in sticking to and invading the valve leaflets.
The causes are based on the type that is present as follows:
- Infective endocarditis
- Native valve infection: The main microorganisms that are involved in infective inflammation of the heart valve include streptococcus, enterococcus, and staphylococcus species of bacteria.
- Rheumatic valvular disease
- Congenital heart disease
- Mitral valve prolapse
- Degenerative heart disease
- Prosthetic valve endocarditis: The early disease is caused by staphylococcus(MRSA) and late disease is caused by streptococcus
- Local abscess
- Valvular dehiscence
- Fistula formation
- Intravenous drug abuse: Staphylococcus, streptococcus, and pseudomonas bacteria are usually involved. Fungal infections are also common in iv drug abusers
- Nosocomial infective endocarditis: Staphylococcus, Streptococcus, and enterococci are usually involved
- Central and peripheral intravenous catheters
- Hemodialysis shunts
- Chemotherapeutic lines
- Fungal endocarditis: Usually caused by candida Albicans, Histoplasma, and Aspergillus
- Native valve infection: The main microorganisms that are involved in infective inflammation of the heart valve include streptococcus, enterococcus, and staphylococcus species of bacteria.
- Non-infective endocarditis
- Steroid therapy
- Systemic lupus erythematosus
- Cancer
- Antiphospholipid syndrome
- Impaired antithrombotic mechanisms
Risk factors for endocarditis
Individuals with the following risk factors:
- Infective endocarditis
- Presence of artificial heart valves and other intra-cardiac devices
- Unrepaired congenital heart defects
- Chronic rheumatic heart disease
- History of inflammation of the heart valve
- Age-related heart valve damage
- Diabetes
- Hypertension
- HIV/AIDS
- IV drug abuse
- Prolonged hospital stay
- Treatment with immunosuppressant agents
- Non-infective endocarditis
- Hypercoagulable states and coagulopathies
- Catheter bases trauma
- Prolonged steroid therapy
- Cancers such as adenocarcinomas
- Autoimmune diseases - SLE
Symptoms & signs
The following are signs and symptoms associated with
- Infective endocarditis
- Fever and chills
- Loss of appetite
- Weight loss
- Weakness and fatigue
- Night sweats
- Joint and muscle pains
- Cough
- Shortness of breath
- Chest pain
- Signs and symptoms of heart failure
- Abdominal symptoms such as pain, vomiting and discomfort after meals
- Janeway Lesions: Red spots on the soles of the feet or the palms of the hands
- Osler’s nodes: Red and tender spots under the skin of the fingers and toes
- Petechial hemorrhages in the eyes, skin, mouth
- Non-Infective Endocarditis is mostly asymptomatic, but symptomatic individuals may show:
- Symptoms and signs of heart failure: Breathlessness on exertion, breathlessness at rest, weakness, swelling of the feet, ankles, and legs, and swelling of the abdomen.
- Symptoms and signs of cerebrovascular embolism: Focal or generalized weakness, numbness, vision loss, speech disturbances, gait disturbances, difficulty swallowing, and memory loss.
- Symptoms and signs of systemic thromboembolism: Pain, vomiting, coldness, and numbness of the arms and feet.
- Symptoms and signs of secondary infections: Fever, chills, cough, breathlessness, chest pain.
Investigations
Some investigations that may be included:
- For infective endocarditis -
- Laboratory tests
- CBP & ESR
- Basic metabolic panel
- Liver and renal function tests
- Rheumatoid factor
- Complete urine examination
- Blood culture
- Imaging tests
- Chest x-ray
- Echocardiography: 2d, doppler, transthoracic echo, a trans-esophageal echo
- Ventilation-perfusion scanning
- Electrocardiography
- Cardiac catheterization: To determine the degree of valvular damage
- Laboratory tests
- For non-infective endocarditis
- Laboratory tests
- CBP & ESR
- Blood culture
- Coagulation profile
- Basic metabolic panel
- Antiphospholipid antibody test
- Antinuclear antibody test
- Anti-DNA antibody test
- Imaging tests
- Chest x-ray
- Echocardiography: Transthoracic echo and transesophageal echo
- Coronary angiography
- Cardiac catheterization
- Laboratory tests
Diagnosis
A diagnosis is established based on medical history, clinical evaluation, and results of the investigations done.
Treatment options
The treatment depends on the type and underlying cause and usually includes medical management and surgical interventions if required.
Medical management
Medical management of endocarditis may include the following:
- For infective endocarditis
- Antibiotic therapy: To control and eliminate the infections
- Heart failure if present, needs to be managed as well
- For non-infective endocarditis
- Anticoagulation therapy:Warfarin may be required if there is SLE
- Antibiotic therapy: For prophylaxis against or if there is a presence of secondary infective endocarditis
Interventional including surgery and indications for surgery
Interventions for the management may include surgical interventions. It requires surgery if the following are present.
- Congestive heart failure refractive to medical therapy
- Fungal Infective inflammation of the heart valve
- Persistent sepsis after 72 hours of antibiotic therapy
- Recurrent septic emboli, even after 2 weeks of antibiotic therapy
- Septal abscess causing a disturbance in electrical conduction
- Intracardiac fistula
- Infected devices
Role of Diet/Exercise/Lifestyle changes/ Preventive
Some measures that may help in reducing the risks are:
- Prophylactic antibiotic therapy before surgical or dental procedures for individuals with cardiac devices, history of cardiac surgeries, or history of inflammation of the heart valve.
- Maintaining good hand and respiratory hygiene.
- Avoiding recreational drug use.
Complications
Some of the complications are included:
- Heart valve damage
- Heart failure
- Seizures
- Stroke
- Cerebral infections and abscess
- Pulmonary embolism
- Kidney failure
- Spleen damage
- Death
Prognosis
The prognosis of endocarditis is generally good with early detection and management, however, it is also dependent on the underlying cause, comorbidities, and the general health of the individual.
When to contact the doctor or hospital/how to identify the emergency or complications
It is advisable to seek immediate medical attention if symptoms and signs of endocarditis are noticed, especially in individuals with a history of cardiac disease or cardiac devices.
Indications for hospitalization if required
Hospitalization may be required for the management of endocarditis especially if surgical interventions are required.
Screening methods
Periodic cardiologic evaluations and consultations are recommended in individuals with implanted cardiac devices.
Suggested clinical specialist/departments to consult for this condition
This will be treated by specialists from the department of cardiology.
Was this article helpful?
YesNo




