Allergy
Blood Diseases
Bone & Joints
Brain
Cancer
Child Care
Cosmetic Surgery
Diabetes
Endocrinology
ENT
Eye
Gen Medicine
General Surgery
Heart
Kidney
Lifestyle
Liver & Digestive
Lung
Men’s Health
Mental health
Physiotherapy
Rheumatology
Skin and hair
Sleep Disorders
Spine
Transplant
Women Health
Thyroid
Vascular Surgery
Basal Cell Cancer of the skin
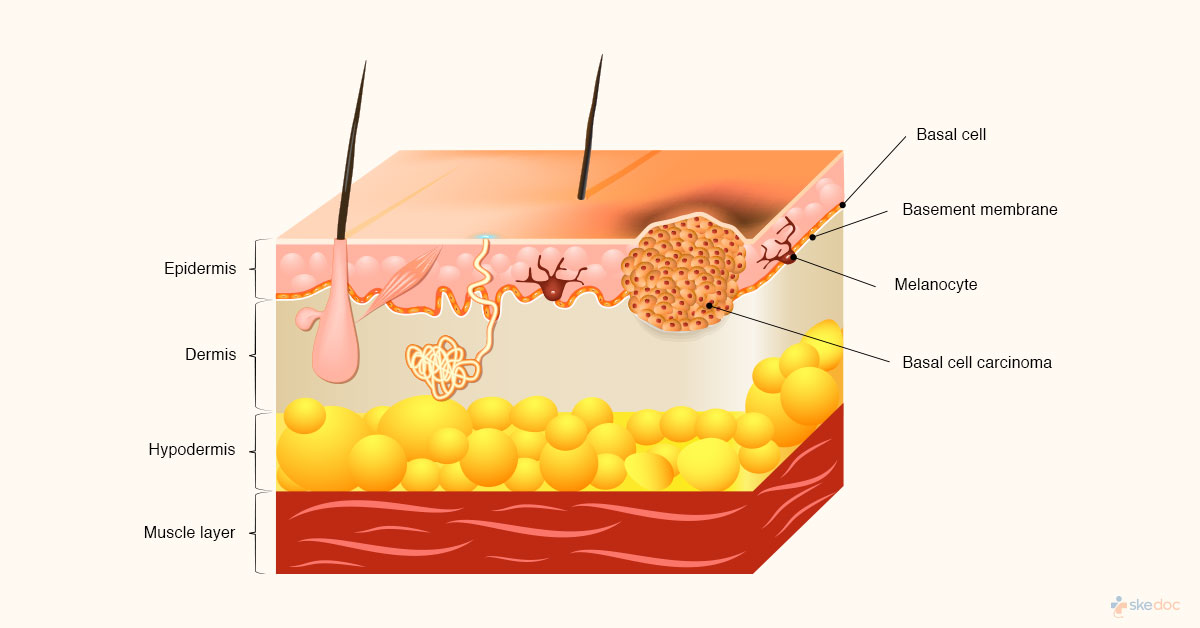
What Is Basal Cell Skin Cancer?
Basal Cell Skin Cancer of the skin is cancer that develops from the cells that line the lower layers of the epidermis of the skin. Basal cell carcinoma is slow-growing and locally invasive cancers that mostly appear on the areas of skin that are exposed to the sun such as the face, head, and neck with only a few seen on the trunk or extremities.
Alternate names
Rodent ulcer, Basilioma, Basal Cell Cancer, Basal Cell Carcinoma, Non-Melanoma Skin Cancer
Is this condition a medical emergency?
Basal cell cancer of the skin is not a medical emergency, however, early detection and treatment are essential in the management of this condition.
Types of this condition
Basal Cell Skin Cancer may be of the following types
- Nodular basal cell cancer of the skin: Most common BCC, seen as round flesh-colored with prominent blood vessels
- Infiltrative basal cell cancer of the skin: The BCC infiltrates the deeper layer and is not very visible clinically
- Micronodular basal cell cancer of the skin: This type of BCC has a well-defined border, is hard to touch, and does not ulcerate
- Morpheaform basal cell cancer of the skin: This type of BCC is ls flat or depressed, firm and waxy to touch, white or yellow
- Superficial basal cell cancer of the skin: This type of BCC is seen usually on the shoulders or the trunk is like a whitish scaly plaque
What causes basal cell skin cancer
The exact cause for basal skin carcinoma is not known but genetic and environmental factors are known to play a role in its development. Excessive exposure to the sun and ultraviolet light can result in the mutation and multiplication of these mutated basal cells of the epidermis leading to basal cell cancer of the skin. They are also most commonly seen in regions where there are hair follicles and sebaceous glands. Although they mostly arise from the outer layer of the skin, they may also arise from the hair follicles.
Risk factors
Some risk factors for the development of Basal Cell Skin Cancer include
- Elderly age group and male gender
- Prolonged exposure to the sun
- Higher altitude regions
- Radiation exposure
- History of skin cancer
- Fair skin and hypopigmentation
- Immunosuppressant therapy
- Exposure or ingestion of arsenic
- Genetic diseases that predispose to cancer such as Nevoid basal cell carcinoma syndrome, xeroderma pigmentosum, Oley syndrome, BDC syndrome, Rombo syndrome
- Previous cutaneous injury – such as cutaneous lupus, sebaceous naevus
- Excessive alcohol consumption
- They may also be seen in association with squamous cell carcinoma, seborrheic keratosis, actinic keratosis
- Type of skin – very fair-skinned individuals, and albinos are at a greater risk
Basal Cell Skin Cancer symptoms & signs
The symptoms and signs of basal carcinoma may include the following depending on the type of basal cell cancer that is present
- Slow growing growths
- A waxy raised area of skin with a central depression
- Pearly appearance
- Irregular borders
- Ulceration or erosion usually in the center
- Bleeding, mostly with minor trauma
- Crusting
- Raised borders
- Translucent lesions
- Tiny blood vessels may be seen on the surface
- The color may vary from skin-colored, light brown, pink, or blue or black pigmentation
Investigations
Some investigations that may be done for establishing a diagnosis of basal cell cancer of the skin include the following
- Skin biopsy
- Punch biopsy or excision biopsy
Diagnosis
A diagnosis of basal skin cancer is established based on medical history, clinical evaluation, and results of the investigations done. Based on the histologic examination this is divided into differentiated and undifferentiated BCC. The micronodular and the morphea from basal cell cancer are considered aggressive skin cancers that can spread to other parts of the body.
Course & stages if any
The staging of basal skin cancer is as follows
- Stage 0: cancer involves the epidermis and has not spread to the dermis
- Stage I: cancer is less than 2cm and has not spread to the lymph nodes
- Stage II: cancer is more than 2cm, but has not spread to the lymph nodes or other organs
- Stage III: cancer has spread to the tissues beneath the skin (such as the muscles, bone, or cartilage) and the lymph nodes, but has not spread to the distant organs
- Stage IV: Basal Cell Skin Cancer metastasis has occurred and cancer has spread to distant organs
This is also categorized as a high-risk tumor if any of the following are present
- If it is a recurrent or incompletely excised tumor
- If it has indistinct borders
- Lesions in high risk, cosmetically important, or functional areas such as
- Basal cell carcinoma on eyelids
- Basal cell carcinoma on the nose
- Basal cell carcinoma on ears
- Basal cell carcinoma on the upper lip
- Basal cell carcinoma on scalp, temples, or face
- Basal cell carcinoma on genitals, and perianal region
- Fast-growing tumors
- Tumors that develop in sites of the previous radiotherapy
- Tumors in immunosuppressed individuals
Basal Cell Skin Cancer treatment options
The treatment of basal skin carcinoma is aimed at the elimination of the tumor with preservation of function and appearance. Surgical and pharmacological interventions and radiotherapy may be done for the management of basal cell cancer. In almost all cases of basal cell cancer surgery is the primary treatment of choice. For recurrent basal cell carcinomas medical, surgical, and radiation therapy is advised.
Medical management
Medical management of basal cell cancer of the skin may include the following
- Antineoplastic agents: such as 5-Fluorouracil, via local chemotherapy, is useful in some type BCC such as small and superficial tumors
- Hedgehog Pathway Inhibitors: such as vismodegib
- Keratolytic agents: such as tazarotene
- Topical skin applications: such as Imiquimod
- Nicotinamide
Interventional including surgery and indications for surgery
Interventional management of basal skin carcinoma may include the following
- Excision biopsy: The lesion is cut and removed
- Mohs Micrographically Controlled Excision: Layer by layer excision while monitoring under a microscope to ensure complete removal. It is indicated in the following cases
- Presence of traumatic scars
- Previously irradiated skin
- Areas of chronic inflammation, ulceration, or osteomyelitis
- Individuals with genetic conditions that predispose to skin cancers
- Curettage and Electrocautery: Excision followed by application of heat for low-risk BCC
- Cryotherapy: The lesion is exposed to extremely cold temperatures; it is indicated for low-risk BCC
- Photodynamic therapy: The lesion is treated with a photosensitive chemical and is then exposed to light, which destroys the tumor cells
Radiation
Radiotherapy may be used for the management of basal cell cancer of the skin, as this basal carcinoma is sensitive to radiation. It may be done as a primary treatment or as an adjunct to surgical intervention. It is usually done in individuals who cannot undergo surgery. The treatment is done over a few weeks. It is not advised in individuals who are otherwise at high risk for developing skin cancer. It is also preferred for the management of basal cell carcinomas in functional and cosmetically challenging areas of the body
Role of diet/exercise/lifestyle changes/ preventive
Some measures that may be taken to reduce the risk of basal skin cancer include
- Avoid excessive exposure to the sun
- Wear protective clothing or gear if working in the sun
- Use high SPF and broad-spectrum sunscreens when going outdoors
- Avoid the use of indoor tanning equipment
Complications
Some complications that may be associated with basal skin cancer include
- Recurrence of basal cell cancer
- Metastasis and involvement of distant organs
- Increased risk of other types of cancer
Prognosis
The prognosis for basal cell cancer is excellent, especially if cancer has not spread to other areas, and if it is detected and treated early.
When to contact the doctor or hospital/how to identify the emergency or complications
It is advisable to seek medical attention if a growth on the skin is noticed, especially if it is bleeding, non-healing, and growing either slowly or rapidly over time.
Indications for hospitalization if required
Hospitalization is not required for basal skin carcinoma.
Screening methods
A dermatological screening and examination once in 3 years are advisable for all high-risk individuals in the age group of 20-40 years and screening and examination every year for those above the age of 40 years.
Suggested clinical specialist/departments to consult for this condition
Basal cell carcinoma of the skin will be treated by specialists from the Department of Dermatology.
Was this article helpful?
YesNo




